During the Coronavirus pandemic, the Centers for Medicare and Medicaid Services (CMS) has taken unprecedented action to expand telehealth for Medicare beneficiaries. Since people were advised to stay at home to reduce risk of exposure of COVID-19, there was an urgency to increase access to telehealth services to help people who need routine care and allow beneficiaries to remain in their homes. Early CMS data have shown telehealth to be an effective way for people to access Home Health Care Service safely during the COVID-19 pandemic, whether it’s getting a prescription refilled, managing chronic conditions, or obtaining mental health counseling.
Today, we share data highlighting the impact of telehealth on beneficiary access. We also discuss how we are using this information to assess whether these expanded telehealth policies should remain in place beyond the COVID-19 public health emergency.
Telemedicine—which includes telehealth and other virtual services—allows patients to visit with clinicians remotely using virtual technology. Innovative uses of this kind of technology in the provision of Home Health Care Service are increasing with advances in telehealth platforms and remote patient monitoring technology. New mobile health apps and wearable monitoring devices help track a patient’s vitals, provide alerts about needed care, and help patients access their physician. CMS has long prioritized telemedicine innovation, but COVID-19’s emergence in the U.S. prompted us to drastically accelerate our efforts.
On March 13, 2020, President Trump made an emergency declaration under the Stafford Act and the National Emergencies Act, empowering CMS to issue waivers to Medicare program requirements to support Home Health Care Service providers and patients during the pandemic. One of the first actions CMS took under that authority was to expand Medicare telehealth on March 17, 2020, allowing all beneficiaries to receive telehealth in any location, including their homes. Subsequently, CMS announced additional temporary rules and waivers to expand the scope of Medicare telehealth services, making it easier for more types of health care providers to offer a wider range of telehealth services to beneficiaries across the country. CMS observed immediate, dramatic increases in telehealth services.

With these transformative changes unleashed over the last several months, it’s hard to imagine merely reverting to the way things were before. As the country re-opens, CMS is reviewing the flexibilities the administration has introduced and their early impact on Medicare beneficiaries to inform whether these changes should be made a permanent part of the Medicare program.
CMS Actions To Expand Telemedicine Before COVID-19
By law, Medicare can only pay for most telehealth services in limited circumstances: when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the telehealth service. A telehealth service must use an interactive audio and video telecommunications system that permits real-time communication between the distant site practitioner who is remotely furnishing the service—such as a physician, nurse practitioner or physician assistant—and the patient at a local medical facility.
The Trump Administration recognized the value of telemedicine for patients and home health care providers long before the pandemic, as part of CMS’s Fostering Innovation Strategic Initiative, the agency’s comprehensive strategy to improve patients’ access to emerging technologies. That’s why over the last three years CMS made several changes to improve access to virtual care. We expanded the services that can be delivered via telehealth, adding services such as wellness visits that require additional time for complex patients and care for patients experiencing a stroke or with End Stage Renal Disease.
In 2019, Medicare started paying for brief communications or Virtual Check-Ins, which are different from traditional Medicare telehealth visits as they are brief patient-initiated communications with a health care practitioner and not limited to patients residing in rural areas. Medicare also started paying for similar virtual communications with clinicians at Rural Health Clinics and Federally Qualified home health care providers, expanding access to care for patients in underserved rural areas.
And starting in 2020, Medicare separately has paid clinicians for e-visits, which are non-face-to-face, patient-initiated communications through an online patient portal. These types of services don’t require Medicare patients to go to the doctor’s office and are available in all types of locations including the patient’s home, and in all areas of the country (not just rural areas). Beneficiaries need to have an established or existing relationship with their Home Health Care Service provider to get these virtual services.
Similarly, CMS implemented statutory changes enacted by Congress so that Medicare Advantage (MA) plans have the flexibility to offer innovative telehealth services as part of their basic benefit, expanding access to the latest telehealth technologies for MA enrollees. In 2020, over half of all plans are offering these additional telehealth benefits, reaching approximately up to13.7 million Medicare Advantage enrollees.
Expanding Telemedicine For Medicare Beneficiaries During The COVID-19 Outbreak
CMS’s efforts to expand telehealth prior to the COVID-19 public health emergency served as a strong foundation for action in the early days of the pandemic. One of the first steps CMS took in response to the COVID-19 public health emergency was to temporarily expand the scope of Medicare telehealth to allow Medicare beneficiaries across the country—not just in rural areas—to receive telehealth services from any location, including their homes. CMS also added 135 allowable services, more than doubling the number of services that beneficiaries could receive via telehealth. Examples include emergency department visits, initial nursing facility and discharge visits, home visits, and physical, occupational and speech therapy services. Medicare also ensured that Home Health Care Service providers like physicians were paid for these telehealth services at the same payment rate as they would receive for in-person services. Additionally, CMS is allowing telehealth technology to fulfill many requirements for clinicians to see their patients face-to-face in different health care settings, including inpatient rehabilitation facilities, hospice, and home health.

CMS has temporarily expanded the types of Home Health Care Service providers that can offer telehealth to broaden patient access to care. Outside of the public health emergency, only doctors, nurse practitioners, physician assistants, and certain other types of practitioners could deliver telehealth services. During the emergency, a wider range of practitioners can provide telehealth services, including physical therapists, occupational therapists, and speech-language pathologists. Additionally, for the first time, through temporary authority added by the CARES Act, CMS is able to pay Rural Health Clinics and Federally Qualified Health Centers to provide telehealth services, giving Medicare beneficiaries located in rural and other medically underserved areas more options to access care from their home without having to travel.
The Trump Administration has also removed other barriers that may limit beneficiary access to telehealth services. Usually, interactive audio-video technology is required for telehealth visits. This can be a challenge for beneficiaries; often, they either don’t have access to the technology or choose not to use it even if offered by their practitioner. At the beginning of the public health emergency, the Department of Health and Human Services (HHS) Office of Civil Rights announced that it would exercise enforcement discretion and waive penalties for HIPAA violations against Home Health Care Service providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the emergency. Soon after, CMS went even further to eliminate these barriers by paying for certain telephone evaluation and management visits and behavioral health services, and paying practitioners at the same rate as similar in-person services.
In addition, HHS Office of Inspector General announced that it would not enforce requirements for practitioners to collect copayments from patients for these kinds of services.
Unprecedented Increases In Telemedicine
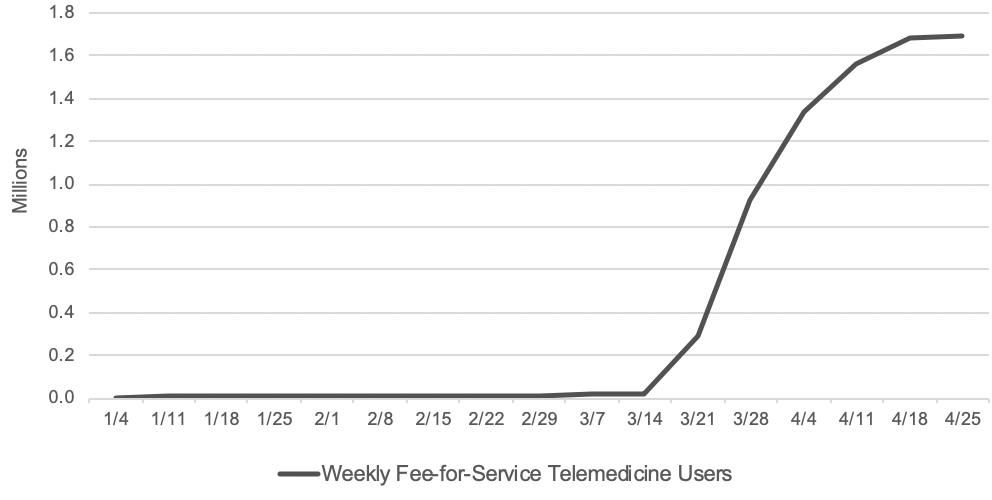
With wide-ranging telemedicine flexibilities, there has been a surge in the number of beneficiaries getting telemedicine services. Before the public health emergency, approximately 13,000 beneficiaries in fee-for-service (FFS) Medicare received telemedicine in a week. In the last week of April, nearly 1.7 million beneficiaries received telehealth services.
In total, over 9 million beneficiaries have received a telehealth service during the public health emergency, mid-March through mid-June. Specifically, data points presented in this section of the post are from internal CMS analysis of Medicare FFS claims data from March 17through June 13, 2020 (using data processed through June 19, 2020). Telemedicine services include services on the Medicare telehealth list including audio-only visits, as well as virtual check-ins and e-visits.
According to Medicare FFS claims data, beneficiaries, regardless of whether they live in a rural or urban area, are seeking care during the pandemic through telemedicine services. In rural areas, 22 percent of beneficiaries used telehealth services, and 30 percent of beneficiaries in urban areas did so. There has been regional variation in use of telemedicine during the pandemic. For example, beneficiaries in northeastern states—New Jersey, Connecticut, Maryland, Delaware, Rhode Island and Massachusetts—have a higher percentage of telemedicine services (over 35 percent of beneficiaries in those states received a telehealth service) compared to those in states in the north central part of the country—South Dakota, Nebraska, North Dakota, Montana and Idaho (less than 17 percent of beneficiaries in those states received a telehealth service). The regional variation could be due to the extent to which Home Health Care Service providers in those states offered telemedicine services and whether patients sought out care via that option.
Beneficiaries are getting care through telemedicine during the pandemic at similar rates across demographics. For example, 30 percent of female beneficiaries and 25 percent of male beneficiaries have received telemedicine services during the COVID-19 public health emergency to date. Across all age groups, 25-34 percent of beneficiaries have received a telemedicine service (34 percent among beneficiaries below the age of 65, 25 percent among beneficiaries between ages 65-74, 29 percent among beneficiaries between ages 75-84, and 28 percent among beneficiaries older than 85). There are also no significant differences by race or ethnicity among beneficiaries who received telemedicine services (25 percent among Asians, 29 percent among Blacks, 27 percent among Hispanics, 28 percent among Whites, and 26 percent among others).
Dually eligible beneficiaries (low-income beneficiaries that qualify for both Medicare and Medicaid) have had higher rates of telemedicine use: 34 percent of dually eligible beneficiaries have had a telemedicine service, compared to 26 percent of Medicare-only beneficiaries. Even among dually eligible beneficiaries, there are no significant differences across race or ethnicity groups (30 percent among Asians, 34 percent among Blacks, 33 percent among Hispanics, 35 percent among Whites, and 31 percent among others).
Evaluation and management (E/M) visits, or office visits, have been the most common form of telehealth, with nearly 5.8 million beneficiaries receiving an E/M telehealth visit since the public health emergency started. Additionally, 38 percent of beneficiaries who had an E/M visit furnished during the public health emergency did so via telehealth. Another area where telehealth has been used frequently has been mental health services with a psychiatrist or psychologist: approximately 460,000 beneficiaries (or 60 percent) receiving this care through telehealth. Telehealth for mental health care is showing great promise for our Medicare beneficiary population, who may otherwise have felt stigmatized seeking out care in-person.
Additionally, during the pandemic, CMS expanded the availability of telehealth services in other settings of care, including nursing homes, where beneficiaries may be particularly vulnerable. We found that 26 percent of beneficiaries who received nursing home visits did so by telehealth. Lastly, nearly 1.5 million beneficiaries have been able to access preventive health services during this time, and 19 percent of those beneficiaries received such services by telehealth.
The use of audio-only telehealth services has also been shown to be helpful for the Medicare population during the public health emergency, as many patients may not have access to or feel comfortable using video technology. Over 3 million beneficiaries have received telehealth services via traditional telephone. That means nearly one-third of beneficiaries that received a telemedicine service did so using audio-only telephone technology.
The claims data are preliminary since Home Health Care Service providers have 12 months after they furnish a service to submit their claims to CMS. But as exhibit 1 shows, the early data show a dramatically accelerated adoption of telehealth in a matter of months, which warrants consideration of which telehealth flexibilities should become a permanent part of the Medicare program.
Exhibit 1: Number of Medicare FFS beneficiaries receiving telemedicine per week
Source: Internal CMS analysis of Medicare FFS claims data, March 17, 2020 through June 13, 2020(using data processed through June, 19, 2020) Notes: Telemedicine is defined to include services on the Medicare telehealth list including audio-only visits, as well as virtual check-ins and e-visits.
Looking Ahead
Telehealth will never replace the gold-standard, in-person care. However, telehealth serves as an additional access point for patients, providing convenient care from their doctor and health care team and leveraging innovative technologies that could improve health outcomes and reduce overall health care spending. The rapid explosion in the number of telehealth visits has transformed the health care delivery system, raising the question of whether returning to the status quo turns back the clock on innovation.
The data have shown that telehealth can be an important source of care across the country, not just for those living in rural areas. Additionally, the immediate uptake in telehealth demonstrates the agility of the health care system to quickly scale up telehealth services, so that Home Health Care Service providers can safely take care of their patients while avoiding unnecessary exposure to the virus.
In light of our new experience with telehealth during this pandemic, CMS is reviewing the temporary changes we made and assessing which of these flexibilities should be made permanent through regulatory action. As part of our review, we are looking at the impact these changes have had on access to care, health outcomes, Medicare spending, and impact on the health care delivery system itself.
First, it is important to assess whether the mode of telehealth service delivery is clinically appropriate and safe for patients, as compared to an in-person visit. For example, during the public health emergency, CMS expanded certain telemedicine services to both new and established patients, where previously those services were limited to patients who had an established relationship with the practitioner. CMS took this action to make these services as widely available as possible given the need to reduce exposure risks for practitioners and patients. As the health care system enters a new normal, it is important to consider whether allowing people with particularly acute needs to be seen by a clinician for the first time via telemedicine, instead of in-person, will result in the best possible outcomes.
Second, we need to assess the Medicare payment rates for telehealth services. During the public health emergency, Medicare paid the same rate for a telehealth visit as it would have paid for an in-person visit, given the unique circumstances of the pandemic. Outside the pandemic, by law Medicare usually pays for telehealth services at rates similar to what professionals are paid in the hospital setting for similar services. Further analysis could be done to determine the level of resources involved in telehealth visits outside of a public health emergency, and to inform the extent to which payment rate adjustments might need to be made. For example, supply costs that are typically needed to enable safe in-person care (for, e.g., patient gowns, cleaning, or disinfectants) and built into the in-person payment rate are not needed in a telehealth visit. On the other hand, there are new processes that clinicians must create for telehealth visits, with associated costs.
Lastly, it is vital that beneficiaries and taxpayer dollars are protected from unscrupulous actors. As more Home Health Care Service providers use telehealth to treat beneficiaries, CMS is examining our data from many angles. We are monitoring program integrity implications such as practitioners who may be offering shorter telehealth visits with patients to maximize payment, or billing more visits than are possible in a day. We know the path forward to expanding telehealth relies on CMS addressing the potential for fraud and abuse in telehealth, as we do with all services.
During these unprecedented times, telemedicine has proven to be a lifeline for Home Health Care Service providers and patients. The rapid adoption of telemedicine among providers and patients has shown that telehealth is here to stay. CMS remains committed to ensuring that the government supports innovation in telehealth that leverages modern technology to enhance patient experience, providing more accessible care.
By Seema Verma | July 15, 2020
Source: Health Affairs