The COVID-19 pandemic and killing of George Floyd along with other recent deaths of African American people at the hands of police have laid bare stark structural and systemic racial inequities and their impacts on the health and well-being of individuals and communities. While these events have brought health and health care disparities into sharp focus for the media and public, they are not new. These longstanding and persistent health disparities are symptoms of broader social and economic challenges that are rooted in structural and systemic barriers across sectors — including housing, education, employment, and the justice system — as well as underlying racism and discrimination. Amid this difficult time for our nation, the increased recognition and understanding of disparities could provide a catalyst for the challenging work required to address them.
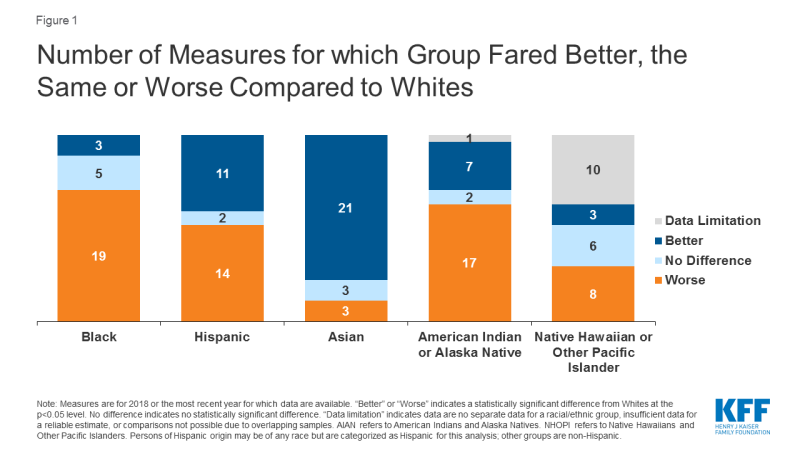
Despite being recognized and documented for many years, disparities in health and health care have persisted and in some cases widened over time. Our analysis finds that Black and American Indian or Alaska Native (AIAN) individuals continue to fare worse compared to White individuals across most examined measures of health status, including physical and mental health status; birth risks; infant mortality rates; HIV and AIDS diagnosis and death rates; and prevalence of and death rates due to certain chronic conditions (Figure 1). For example, the infant mortality rate for Black and AIAN individuals is roughly two times higher than the rate for White individuals. Black teens and adults have an over eight times higher HIV diagnosis rate and a nearly ten times higher AIDS diagnosis rate compared to their White counterparts; the HIV and AIDS diagnosis rates for Hispanic teens and adults are more than three times higher compared to the rates for those who are White.
The disparate impacts of the COVID-19 pandemic on people of color mirror and compound these broader underlying racial/ethnic disparities in health. Data across states show that, in the majority of states reporting data, Black people account for a higher share of COVID-19-related deaths and cases compared to their share of the population. Similarly, Hispanic individuals make up a higher share of confirmed cases relative to their share of the population in most states reporting data, and there have been striking disproportionate impacts for American Indian or Alaska Native, Asian, and Native Hawaiian or Other Pacific Islander people in some states. The resulting economic crisis has also had an unequal effect on people of color.
Health disparities, including disparities related to COVID-19, are symptoms of broader underlying social and economic inequities that reflect structural and systemic barriers and biases across sectors. Though health care is essential to health, it is a relatively weak health determinant. Research shows that social determinants of health—the conditions in which people are born, grow, live, work and age—are primary drivers of health. They include factors like socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care (Figure 2). For example, children born to parents who have not completed high school are more likely to live in an environment that poses barriers to health such as lack of safety, exposed garbage, and substandard housing. They also are less likely to have access to sidewalks, parks or playgrounds, recreation centers, or a library. Further, evidence shows that stress negatively affects health across the lifespan and that environmental factors may have multi-generational impacts.
The heightened focus on and understanding of disparities can serve as a catalyst for the challenging work required to address them. Steps can be taken within the health care system that would help address health disparities. For example, actions to expand health coverage, such as adoption of the Medicaid expansion to low-income adults in the 14 states that have not yet expanded; increasing accessibility to health care providers; increasing access to linguistically and culturally appropriate care; and diversifying the health care workforce could help reduce health disparities. However, efforts to address health disparities also require cross-sector approaches beyond health care to affect the broader social and economic factors driving health. For example, actions to increase access to healthy food options and improve food security; improve affordability and quality of housing; enhance educational opportunities; improve built environments and provide more green spaces and recreational opportunities; and increase financial security and economic opportunity may all positively affect health and reduce health disparities. Beyond these factors, any effort would be woefully incomplete if it does not also recognize and address racism and discrimination and long histories of stress and trauma affecting the health of individuals and communities and how they shape our systems and policies. Such efforts are challenging and complex and require strong leadership, community engagement, resources, and cross-sector collaboration to achieve progress forward.